Making Mental Health Tangible: Chronic Stress and the Brain
December 14, 2018Does your work involve caring for or supporting others? If you’re exposed to other people's suffering on a regular basis, you're at risk of experiencing compassion fatigue (CF), a.k.a. secondary traumatic stress (STS).
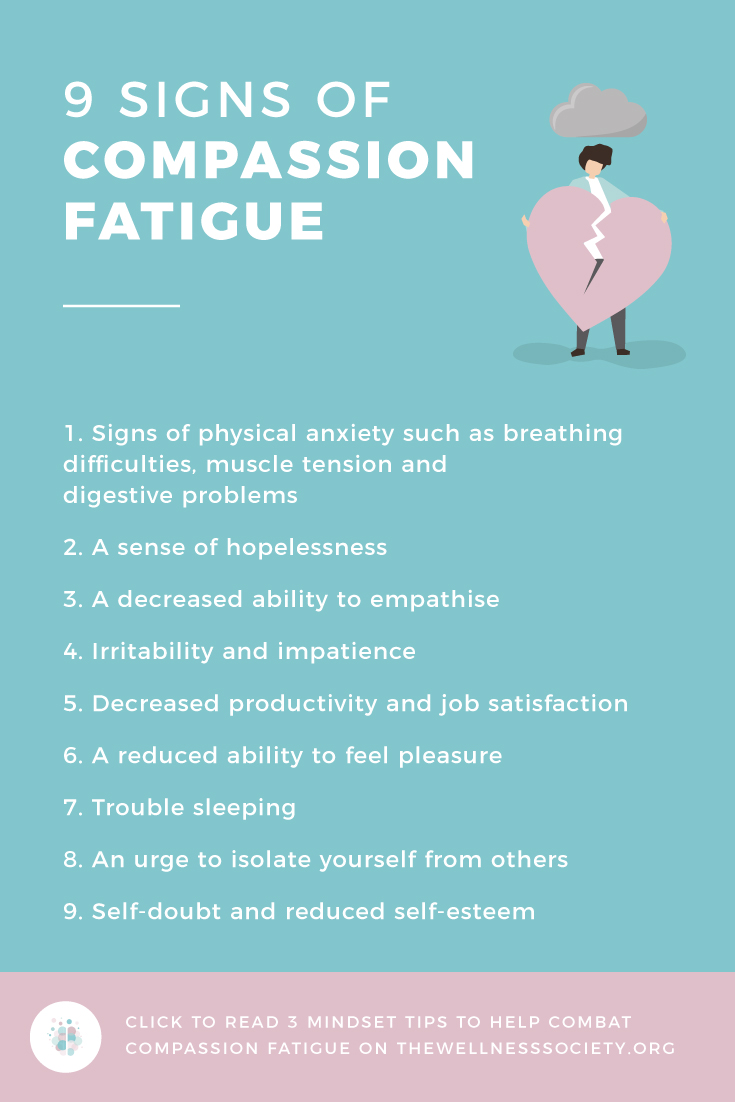
Common signs of compassion fatigue include:
- A sense of hopelessness
- Decreased ability to empathise
- Irritability and impatience
- Decreased productivity and job satisfaction
- A reduced ability to feel pleasure
- Trouble sleeping
- An urge to isolate yourself from others
- Self-doubt and reduced self-esteem
- Signs of anxiety such as breathing difficulties, muscle tension and digestive problems
If you think you might be suffering from compassion fatigue, you can take the Professional Quality of Life Scale Screening test (PROQOL) – it’s available to download for free here.
It’s important to note that compassion fatigue is a normal human response commonly seen in empathetic people. It isn’t a disease or an illness. It’s a temporary state, a spectrum, that you can shift further out of.
So, how can you deal with compassion fatigue? Your mindset plays a big role. Five factors associated with compassion fatigue are:
- High expectations of work
- Idealistic worldviews
- The view that self-care is selfish
- A lack of strong personal boundaries
- An overdeveloped sense of responsibility
With the above in mind, here are three mindset shifts to help you feel better.
1. “I’ll See the Good Whilst Accepting the Bad”
"Sometimes in life we must fight not only without fear, but also without hope.” – Alessandro Pertini
Perhaps you were drawn to your job due to a strong desire to make a difference in the world. Sadly, this can be met with a sense of disillusionment and hopelessness after being exposed to tragedy and suffering that you have little control over.
How much time do you spend focusing on things that you can't change? The highly empathetic, passionate and sensitive people susceptible to compassion fatigue often feel as though they’re carrying the whole weight of the world on their shoulders.
Letting go of this overdeveloped sense of responsibility can be truly life-changing. To help you make this mindset shift, it can be helpful to bring to mind the Serenity Prayer:
"Grant me the serenity to accept the things I cannot change, courage to change the things I can, and wisdom to know the difference."
Suffering is, and always will be, universal. Developing mental resilience is how we handle this difficult fact of life. Mental resilience is reminding ourselves that positive outcomes are not always achievable. It’s accepting our human limitations and letting go of perfectionism. It’s reframing thoughts and situations in the most helpful way possible.
It’s seeing the good by not overlooking the “small” ways in which you help every single day – just by being there, offering a listening ear, and reminding vulnerable clients that caring people exist.
When you focus on developing mental resilience, you make space for what’s called ‘compassion satisfaction’, the feeling of joy and contentment you get from making a difference.
2. “Self-Care is Essential to Mental and Physical Health”
Helping-oriented people often view self-care as a form of self-indulgence. Perhaps the idea of focusing on yourself makes you feel self-centered and selfish, and fills you with shame.
This view of self-care is a hazard to your health. We urge you to become mindful of this for your mental and physical wellbeing. The body keeps the score when it comes to stress. Self-care is your way of protecting yourself against the dangers of poor mental wellbeing. As Mandy Stevens explains in an article in The Guardian, rising stress levels can creep up on us in slow and insidious ways:
“Despite 30 years’ experience as a registered mental health nurse I didn’t recognise, acknowledge or even notice the range of symptoms I had been experiencing, or how they had been affecting me. It was only when I finally cried at work that I realised something was wrong.”
3. “It’s Okay to Set Compassionate Boundaries”
“Compassionate people ask for what they need. They say no when they need to, and when they say yes, they mean it. They’re compassionate because their boundaries keep them out of resentment.” – Brené BrownCompassionate boundary setting involves deciding what you will and won’t accept for your wellbeing, and it’s a skill you can get better at over time.
Saying no is a key part of setting compassionate boundaries. When you’re so focused on serving others (as those susceptible to compassion fatigue are), saying no can feel hellish at first. However, those who care for you and respect you will accept your need to step back. Every time you say no when you’re overstretched, you’re honoring your needs and protecting your mental and physical wellbeing.
Another important way to set compassionate boundaries is to ask for help. Beverly Diane Kyer shares her personal experience with this in her book Surviving Compassion Fatigue:
“Helpers typically do not ask for help. Certainly not I. Perhaps hardest, was to reconcile how my service as a helping professional, service that I was called to and passionate about doing, was hurting me. In the past, I could not fathom this and did not realise that I needed to take care of me while taking care of others. I get it now. This is hard work, painful and distressing work. As important as it is, this work comes with a price, and so I need help to do it well and take care of myself in the process.”
If you’re struggling with compassion fatigue, it’s important to tell your supervisor how you're feeling. Ask them what reasonable adjustments they could make to help support your mental health to prevent it from deteriorating further. They may refer you to your Employee Assistance Programme (EAP) or encourage you to explore accessing therapy.
Summary
Recovering from and preventing compassion fatigue begins with awareness and acceptance of your experience. If you notice you’re experiencing the signs of compassion fatigue, adopting these mindsets can help you feel better:
- "I’ll see the good whilst accepting the bad.”
- “Self-care is essential to mental and physical health.”
- “It’s okay to set compassionate boundaries.”
Check out this article for information on how to prevent burnout.
Build Your Mental Wellbeing Toolkit
Want practical tools to prevent compassion fatigue? Check out The Professional's Mental Wellbeing Toolkit today. It's "everything you need all in one place."
Pin This Page